Using Risk Stratification in Patient Engagement Strategies
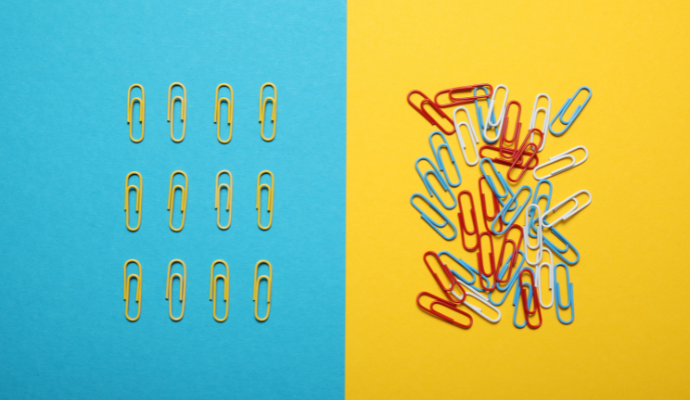
Providers must use risk stratification to better target their patient engagement strategies to patients who need more meaningful health activation.
Source: Getty Images
- As healthcare professionals continue to develop meaningful patient engagement strategies, they should consider using risk stratification to determine how and with which patients providers will engage.
Risk stratification is “the process of assigning a health risk status to a patient, and using the patient’s risk status to direct and improve care,” according to the American Academy of Family Physicians (AAFP).
“The goal of [risk stratification] is to help patients achieve the best health and quality of life possible by preventing chronic disease, stabilizing current chronic conditions, and preventing acceleration to higher-risk categories and higher associated costs.”
Said otherwise, risk stratification helps healthcare providers tailor their patient engagement and care management efforts to individual populations with varying healthcare needs. A patient with no comorbidities might not need a lot of patient engagement at the moment. Meanwhile, someone with multiple complex chronic illnesses might need a high-touch engagement strategy.
Intensive patient engagement for an otherwise healthy patient may not be a great investment for primary care providers operating under tight margins. On the other hand, a low-touch patient engagement strategy could lead to costly acute episodes in the emergency department for complex patients.
READ MORE: Patient Engagement Key to Healthcare Consumerism Post-Pandemic
Healthcare professionals can determine how they will target patient engagement strategies by understanding patient needs and which will require more provider attention. These patient engagement strategies will ideally lead to healthier patients who cost the industry less money.
How to Approach Risk Stratification
In patient engagement, risk stratification means determining which patients are most at-risk of developing a costly condition, of costing the organization money, or of seeing a pre-existing healthcare condition worsen. Providers can use risk stratification to better tailor their patient engagement efforts.
For example, a young and healthy patient will likely not need extensive patient engagement from her provider. This low-risk population will usually benefit from annual check-ups, preventive care, and providers who are openly available on the patient portal and other preferred communication channels for potential health emergencies.
However, a diabetic patient will need more sophisticated patient engagement, complete with strong patient-provider communication, regular check-ups, medication management, and care coordination.
Risk stratification in patient engagement means targeting activation efforts appropriately, according to a report from the Commonwealth Fund.
“The success of population health management depends, in part, on accurately identifying patients at high risk for poor health outcomes as well as preventable and costly health events,” the report authors explained. “Risk-stratification approaches typically focus on clinical markers.”
Healthcare organizations usually use artificial intelligence algorithms leveraging data from the EHR to risk stratify patients. Algorithms might look at:
- Disease state or comorbidities
- Social determinants of health
- Patterns of healthcare utilization
- Patterns of visits to high-cost settings, like the emergency department
Typically, healthcare experts refer to patients as being in one of four risk categories: highly complex, high risk, rising risk, and low risk. Using an algorithm factoring in the above metrics (or other metrics important to the unique heath system) can help providers categorize patients into those categories and then tailor patient engagement strategies.
“With such an approach, a care team can quickly react to different intensities of illness in their panel and proactively manage risk,” researchers wrote in a 2019 Journal of Health Care for the Poor and Underserved article. “This approach allows a multidisciplinary care team to target high- risk patients inside the walls of the clinic and the communities where they live.”
Providers should be aware of patients who move in and out of different risk levels. A patient might have a heart attack one year, placing him in a high-risk category. But by the following year, that patient may have quit smoking and started exercising, moving him down into the rising risk or even low-risk category.
Conversely, a patient can move from rising- to high-risk very quickly. Keeping track of rising-risk patients, and even designing some upstream interventions for that risk category, will be critical to keeping healthcare costs at bay.
Keeping up with those fluctuations will require access to big data in real time.
STRATIFYING PATIENTS BY IMPACTABILITY
As many healthcare professionals look at risk stratification scores for patient engagement, others are looking at a different determinant: impactability scores.
Impactability scores investigate the likelihood of a patient responding positively to a patient engagement intervention. A patient with a high health risk may not have a high impactability score. Looking at an impactability score may help healthcare providers triage their patient engagement efforts and focus on those who are predisposed to having a positive response to interventions.
Moreover, emphasizing impactability could also help bring individuals in lower risk tiers, like no risk and rising risk, to the forefront. This could prevent lower-risk patients from becoming costly high-risk patients.
“Analyzing impactability can help organizations understand where best to focus their resources, and how to identify areas where an organization is ill equipped to address certain patients’ needs,” according to the Center for Health Care Strategies (CHCS). “This concept can help organizations further refine their understanding of which patients are more likely to respond to interventions designed to disrupt their trajectory to becoming high-need, high-cost.”
Creating an impactability model can be challenging, researchers have found. It can be difficult to quantify how a patient will react to a certain preventive care intervention, researchers wrote in a Milbank Quarterly study.
However, some factors to consider include:
- Patterns of high-yield care gaps; these are tangible steps that can improve the health and well-being of the individual
- Patient activation scores
- Patterns of program disenrollment
- Resources and ability to use channels amenable to specific patients (patients receptive to text message outreach will not be a good fit for organizations without text message outreach technology)
“Predictive risk models can help identify patients who are truly at risk of future hospitalization,” the Milbank Quarterly study said. “Impactibility models are meant to identify the subset of at-risk patients who are likely to benefit from ‘upstream’ care.”
Of course, impactability and risk scores may beg the question: who gets excluded from the intervention? Although some experts told the Milbank Quarterly researchers that extremely high-risk patients may be excluded from upstream interventions because they are too complex and may have died before seeing outcomes, others argue the contrary.
“Most interviewees felt very high-risk patients should, in general, be offered upstream care,” the researchers wrote. “Because these patients have the highest expected rates of hospitalization, the potential payback for success also is the greatest here.”
Ensuring the right patient receives the right intervention at the right time is the end goal of patient engagement. Determining how much of a clinical or financial risk a patient will pose to a healthcare organization will be important for determining who receives more extensive patient engagement efforts.
Ultimately, this will lead to healthcare efficiency. Providers will be more efficient about where they spend their labor.
Additionally, it will result in a lean patient engagement effort organization-wide. Providers will also reduce healthcare costs by engaging their high-risk patients, keeping those patients healthier and reducing unnecessary or inappropriate healthcare utilization.
